Decker faculty innovate to teach during the pandemic
Earlier this year, most schools and universities worldwide quickly shifted to online learning (at least temporarily) in an attempt to halt the transmission of COVID-19.
A few months later, the good news is that online teaching is now flourishing and has become a practicable alternative to traditional, face-to-face teaching and learning. One of the difficulties, however, is effectively teaching activity-based, lab-based and hands-on courses.
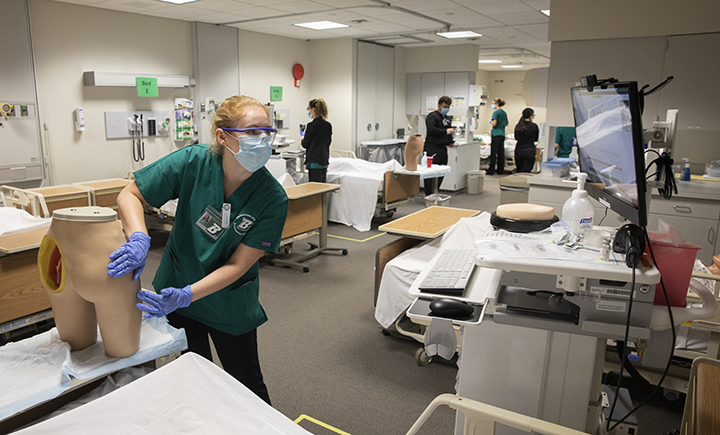
At Binghamton University’s Decker College of Nursing and Health Sciences, nursing faculty are addressing this challenge, sometimes in unexpected ways.
Take the idea of using an inflatable Halloween prop to help students learn patient assessment. This was the brainchild of Lori Sprague, assistant director of Decker College’s Innovative Simulation and Practice Center (ISPC) and a clinical assistant professor of nursing.
“The idea came to me in March or April, after Binghamton sent students home for the rest of the spring semester. ISPC staff and faculty who teach NURS 321 [Nursing Assessment of Clients] were discussing how to teach an online version of the course,” Sprague said. “We knew students would learn more effectively if they had something at home they could practice on; we couldn’t assume everyone would have a live person available to them.”
To master assessment skills, students must learn the process of a head-to-toe assessment as well as understand what they are listening for so they can identify normal versus abnormal sounds (lungs and heart, for example). Then, they must put these skills together while communicating with a patient.
“During the initial in-person labs for NURS 321, a person, inflatable manikin or high-fidelity patient simulator serve the same function by giving landmarks and allowing for repetition of the process,” said Patti Reuther, director of the ISPC.
Reuther and Sprague considered manikins created for instructional purposes, but decided they would be too expensive for students to purchase.
The inflatable manikin — ISPC staff and the course instructors never used or allowed use of the term “doll” — they ultimately decided on was a full-size inflatable body, which is marketed as a Halloween prop and is available for $14.99 on Amazon.com.
While the item is simple, it met all the requirements.
“We were mainly concerned that the manikin we selected was about the size of an adult and had hands and feet so students could demonstrate the proper positioning for pulses,” Reuther said.
Students enrolled in NURS 321 received a communication through the University’s course-management system recommending the purchase of the inflatable manikin and providing links to the preferred item and a few other appropriate choices, all of which were readily available online. It was also discussed during the students’ orientation, and Sprague made a presentation about the use of the inflatable manikin. The students were told that buying the manikin was optional, but most chose to make the purchase.
In addition, students taking NURS 321 have always been required to buy an assessment kit containing a blood pressure cuff, stethoscope, penlight with pupil gauge, bandage scissors and a hemostat (surgical clamp). Reuther knew, however, that students would need additional items at home, so she used part of the simulation fee nursing students pay each semester to purchase practice equipment for each student. This equipment was shipped to the students’ homes and included items for medication administration, changing dressings (bandages) and sterile procedure practice.
Depending on the topic to be covered, faculty would use a high-fidelity manikin in the ISPC to demonstrate the skill (assessment). Then, students would be placed into Zoom breakout rooms in groups of two to practice the skill on their inflatable manikin, with one student giving directions while the second student demonstrated the skill. The students would then switch. The instructors visited the breakout rooms to observe and provide instruction and feedback.
For some assignments, students would be asked to complete specific tasks. They would record themselves completing the task and then submit the videos to their instructor. Instructors would review the recording and provide feedback.
The new way of learning and teaching presented some challenges.
“Getting the students to see the positive experience they were getting was difficult at first,” said Dellazon Gilbert, clinical instructor.
“It was also challenging at times to keep students engaged and have them ‘believe’ that they could learn the content,” added Joyce Rhodes-Keefe, clinical assistant professor. “Some students had considerable doubt they could learn it virtually.”
Despite their initial reluctance, however, students adapted to the remote-learning clinical labs and the use of inflatable manikins.
“If you get students who embrace their education, then they will embrace what you are teaching,” said Gilbert.
“Some students were concerned that they didn’t conduct an assessment/procedure on a live person, but they said they do feel prepared to transfer what they learned on the manikin to an individual,” added Rhodes-Keefe.
Once students returned to campus, they were brought into the ISPC and were able to demonstrate their mastery of the assessment skills. According to Reuther and Sprague, the results were positive.
“Faculty have found the students to be as prepared as prior cohorts who learned in person,” Reuther said.
One area where the students learning at home surpassed classmates who learned solely in the lab is medication administration.
“Previously, we didn’t give students needles and syringes to practice with ahead of time, so they would come into the practice lab and it was a challenge for them,” Sprague said. “Now, they’re practicing the skills at home and their technique is so much better. All the faculty have noticed how well the students handle the syringes.”
Both Reuther and Sprague believe there will be a continued need to teach hands-on skills using an online approach, so they’ve had some preliminary discussions with medical equipment providers to create products better suited to a remote-learning environment.
“Online learning isn’t going away, and we need to get students tools that are both cost-effective and easy to use,” Sprague said.
While a Halloween prop may seem like the most unusual item used in nursing education, the move to online instruction has been the catalyst for some real creativity among clinical nursing faculty.
When faculty and students can’t get to the ISPC, instructors have used various household items to teach clinical nursing skills.
- Gilbert has used hot dogs to teach students how to perform a purified protein derivative (PPD) skin test for tuberculosis.
- Sprague says a plastic disposable cup with a hole in the bottom can be used to help teach catheter placement.
- Rhodes-Keefe and others have augmented teaching using a towel roll for placing blood pressure cuffs, a balloon for demonstrating percussion, fruit for assessing a wound (take a bite from an apple or peach, let it sit for 24 hours and then document how the fruit looks) and even crispy rice cereal for simulating abnormal lung sounds.

