When a person is suffering from alcohol poisoning or a drug overdose, they need immediate help. Learning how to recognize and respond in an alcohol or drug-related emergency can help save lives.
Alcohol emergencies
Know the signs:
- Passed out, unresponsive, or unable to stay conscious
- Fewer than 12 breaths/minute (depressed breathing or irregular pulse)
- Vomiting while passed out
- Cool/clammy skin
- Pale/bluish skin, especially around the lips or under the fingernails
- Inability to walk or lack of physical coordination
- Incontinence
- Seizures
- Confusion or disorientation
When someone is showing these symptoms, they may be at risk of death or permanent injury. Remember that a person does not need to show ALL of these signs to have alcohol poisoning. If you are unsure, call for help.
How to respond:
-
On or off campus, call 911 and put the individual in the recovery position (below)
-
If you dial 911 from a non-campus phone, you will be connected with Broome County 911 and you can ask for Harpur's Ferry
-
If the person may have used opiates in any form, including pain pills, administering Naloxone can reverse an overdose
-
Stay with the person until help arrives and keep the person awake, if possible
-
For people who are conscious and able to swallow, try to get them to slowly drink water
Tip: Add the Harpur's Ferry phone number to your phone now (607-777-3333![]() ) and add it to your favorites list.
) and add it to your favorites list.
Amnesty and good samaritan policies
Binghamton University is committed to promoting the health, well-being and safety of all members of our community. As such, policies have been adopted that are intended to encourage students to seek emergency assistance for oneself or a fellow student regardless of the events occurring at the time the emergency occurred.
Learn more about Binghamton University's amnesty and good samaritan policies.
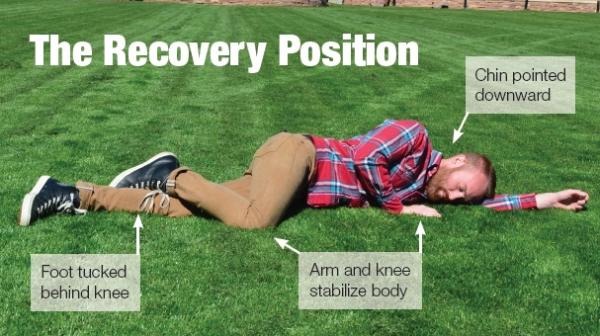
Recovery position
Putting someone in the recovery position (Bacchus Maneuver) will keep the airway clear and open, and ensure that any vomit or fluid won't cause the person to choke. Carefully roll them onto their side with their arm over their head.
- Raise the arm that is closest to you above their head and prepare to roll them towards you onto their side.
- Gently roll them toward you, guarding their head from hitting the floor. The head should rest in front of the arm or leaning up against it and downward.
- While the chin is still pointed towards the ground, tilt it slightly to maintain an open airway. Tuck the nearest hand under the cheek to help maintain head tilt and raise the face of the floor, or place it so that it is stabilizing the body.
View a video on how to put someone in the recovery position.
What not to do:
- Do not attempt to feed the person who could choke on food.
- Do not give the person any other medications; mixing drugs and alcohol will likely make the alcohol poisoning worse.
- Do not force the person to throw up. The person's gag reflex may not work and it could cause choking.
- Do not walk the other person around in an attempt to "walk it off"; reduced physical coordination could lead to falls or other accidental harm.
- Do not put the person in a cold shower; it could lead to hypothermia.
- Do not let the person "sleep it off."
Opioid emergencies
Opioids are drugs derived from opium, also called opiates. They include illicit drugs such as heroin, fentanyl and carfentanyl. Opioids also include prescription pain medications, such as morphine, hydrocodone and oxycodone (Oxycontin).
Opioid overdoses can be fatal and difficult to predict. The best prevention is to avoid opioid use unless explicitly prescribed to you with specific instructions by a medical professional. However, if someone still chooses to use, noting the factors that can contribute to an overdose may help save a life.
Learn more about the Binghamton University Opioid Overdose Prevention Program.
Know the signs:
- Pinpoint pupils
- Shallow breathing or not breathing
- Gurgling, wheezing or snoring sounds
- Blue or grayish lips and nails
- Not responding to stimuli, including pain
Most overdoses occur over a period of 1–3 hours.
How to respond:
- On or off campus, call 911
- If you dial 911 from a non-campus phone, you will be connected with Broome County 911 and you can ask for Harpur's Ferry
- Administer Naloxone (Narcan). Watch a video on how to administer Naloxon
e - If they do not respond, begin CPR
Tip: It is safe to provide Naloxone (Narcan) even if they are not experiencing an overdose, so it is better to be safe than sorry. Naloxone (Narcan) is not a substitute for emergency medical care.
Good Samaritan Law
Some individuals may fear that police will respond to a 911 call and that there will be criminal charges for themselves or for the person who has consumed drugs or overdosed. Those fears should never keep anyone from calling 911 immediately. The New York State 911 Good Samaritan Law allows people to call 911 without fear of arrest if they are having a drug or alcohol overdose that requires emergency medical care or if they witness someone overdosing.
Legal protection
In September 2011, the 911 Good Samaritan Law went into effect to address fears about a police response to an overdose. This law provides significant legal protection against criminal charge and prosecution for possession of controlled substances, as well as possession of marijuana and drug paraphernalia. This protection applies to both the person seeking assistance in good faith as well as to the person who has overdosed. Class A-1 drug felonies as well as sale or intent to sell controlled substances are not covered by the law.
For more information, see the NYS OOPP website.
Campus Code of Conduct protection
No student seeking medical treatment for an alcohol or other drug-related overdose or other life-threatening medical emergency will be subject to University discipline for the sole violation of using or possessing alcohol or drugs. This policy shall extend to another student seeking help for the intoxicated student or the student who is facing a life-threatening medical emergency. In cases of alcohol and prohibitive drug intoxication, the primary concern is the health and safety of the individual(s) involved. For additional information visit the New York State Department of Health website.
Where to get Naloxone
If you are unable to attend a training provided by the Binghamton University OOPP and/or acquire a Naloxone kit, you may seek out another Opioid Overdose Prevention Program in the area or find a local pharmacy that carries Naloxone. Of note, many pharmacies participate in the Naloxone Co-payment Assistance Program (N-CAP), which covers co-payments for naloxone in an amount up to $40 for each prescription dispensed, so in many cases the Naloxone ends up being free. Individuals simply need to request a kit by standing order (i.e. requst a kit without a prescription).
If you are a trained responder in the Binghamton University OOPP and have responded to an opioid overdose, ensure that you complete the initial reporting form in order to acquire a replacement Naloxone kit.
Risk factors for overdose:
- Quality. Substance potency varies substantially and may be cut with dangerous, high-potency opioids.
- Mixing. Mixing opioids, in particular, with alcohol or other medications such as benzodiazepines can slow the respiratory system and stop breathing.
- Tolerance. Tolerance decreases after periods without use including detoxification, hospitalization or if a person resumes use after recovery.
- Environment. Using in isolated environments decreases the likelihood of someone being able to help in an overdose situation.
- Health problems. Underlying health problems, especially chronic lung diseases such as emphysema or sleep apnea, can slow the respiratory system — even when the user is not aware they may have these underlying health problems.